Renée Pellerin is a former CBC health journalist and the author of Conspiracy of Hope, The Truth About Breast Cancer Screening, published by Goose Lane Editions. Below is an except from her article in the Globe and Mail responding to the new guidelines published by the Canadian Task Force on Preventative Health Care for breast cancer screening.
“Every woman over 40 should be aware of new Canadian breast screening guidelines. Every family physician should be prepared to discuss those guidelines with their patients. Every provincial breast screening program should take a good, hard look at what it is telling women.
One of the main harms of screening is false positive results, which can lead to unnecessary further tests including biopsies and the anxiety resulting from being labelled as having cancer. The task force analysis is that false positive results occur in between 20 and 30 per cent of all women screened over seven years.
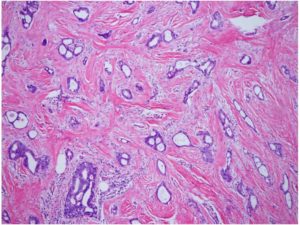
The other main harm is over-diagnosis, not to be confused with a false positive. It’s when a mammogram detects real cancer, but it’s one that does not grow, one that a woman will never feel, will never cause a problem. There is no way to know which screen-detected lesion will behave this way, thus it is always involves surgery and possible additional treatment.
A Canadian screening trial estimated that up to 50 per cent of screen-detected breast cancers in women under 50 were over diagnosed. The number of cases in older women were fewer, but still high. So while screening may discover early cancers that are more easily treated, it may also discover cancers that may be treated unnecessarily.
Yet, how many women and their doctors understand that the benefits of screening are limited, while the risk of over-diagnosis resulting in over treatment is significant?”
Here is the link to the full text from the Globe and Mail on December 11, 2018.
Here is the link to the book Conspiracy of Hope.