Translational research is generally considered a process that starts in the lab—the “bench”—where a new drug, device, or procedure is developed, and ends with the production that makes it available in the clinic—the “bedside.”
Barry S. Coller from the Rockefeller University, NY defines translational medicine as: “The application of the scientific method to address a health need.”
He holds that, in contrast to basic research, which has the generation of new knowledge as its primary goal, the primary goal of translational science is improvement in human health.
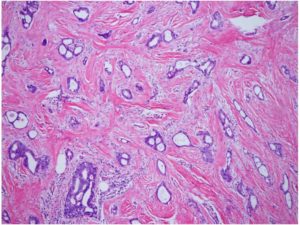
BreastDefense is very close to the “bedside”. The BreastDefense tissue test could be made available to women within a year and the blood test just 24 months later.
“We know more about the human body today than we did yesterday, and tomorrow we’ll know even more—a lot more. In the last two decades, advances in human genome sequencing, molecular imaging, and other areas have sparked a research revolution that reveals ever more detailed and precise information about how our bodies work. Every day brings new discoveries, many of which may hold the potential to improve human health in meaningful ways.
But the pace at which those discoveries lead to improved health has been frustratingly slow. Yes, new drugs and new therapies do reach patients, and when they do, they often make a tremendous difference. But relative to the number of research projects conducted, papers published, and trials run, it is clear that new health care advances have lagged behind the vast amounts of data generated by the explosion in biomedical discovery.
If you look at drug development, the failure rate is over 95 percent,” he says. “So an enormous amount of money is being spent nationwide on things that don’t work.”
This except was taken from Duke Medical Alumni News.
BreastDefense is a simple test that we are confident will work and will quickly have a huge impact on breast cancer survivor rates.